Retinal Detachment Symptoms & Diagnosis
Neighborhood Retina Care Doctors in Sarasota, FL
Retina Specialists Providing Treatment for:
Do I Have a Retinal Detachment?
 Most people will experience a sudden increase in floaters and flashes in their vision sometime between the ages of 50 and 70. A hasty internet search reveals that these symptoms can be associated with a retinal detachment, which can lead to blindness. A feeling of terror sets in as the next internet search is for a local ophthalmologist that has same-day appointments available.
Most people will experience a sudden increase in floaters and flashes in their vision sometime between the ages of 50 and 70. A hasty internet search reveals that these symptoms can be associated with a retinal detachment, which can lead to blindness. A feeling of terror sets in as the next internet search is for a local ophthalmologist that has same-day appointments available.
If you are in this situation, don’t panic but follow this advice before reading the rest of the page. Anyone who is experiencing new flashes and floaters should seek a dilated examination with an ophthalmologist within 24-48 hours. While it is possible that you are in fact experiencing a retinal detachment, the vast majority of patients with these symptoms are not at risk for losing vision. Unfortunately, you cannot be sure that a retinal detachment is not there without an examination by an ophthalmologist.
Retinal Detachment Reviews
If you are experiencing new flashes or floaters in the Sarasota or Manatee area, consider calling our retina specialists at 941-351-1200 to secure a same-day or next-day appointment. We are experts in diagnosing and treating all causes of floaters, retinal tears, or retinal detachments.
What is the Retina?
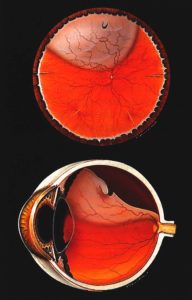
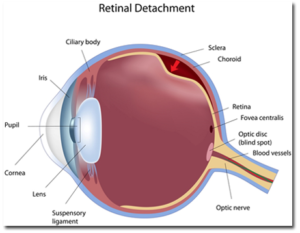
The retina is the light-sensitive layer that lines in the inside, back surface of the eye. The light that enters the eye through the pupil passes through the lens to be focused on the retina. The retina interprets the image and passes the signal along the optic nerve to the brain. Without the retina, there would be no vision.
What is a Retinal Detachment?
A retinal detachment (RD) occurs when fluid forms between the retina and its supporting layers in the back of the eye. While there are multiple ways to develop fluid under the retina, the most common reason has to do with the connection between the retina and the jelly that fills the human eyeball.
Throughout your life, the surface of the retina is in contact with the jelly that fills the eye, called the vitreous. Sometime between the ages of 50 and 70 in most people, the jelly spontaneously pulls away from the retina. We call this a posterior vitreous detachment (PVD). This ‘peeling’ of the jelly from the retina puts tension on the retinal surface. This tension is what causes the flashes that are commonly associated with a PVD.
If the jelly pulls hard enough, or the retina has a preexisting area of weakness, a retinal tear can form. A retinal tear occurs in approximately 5% of vitreous jelly separations. The tear can bleed, which is one common reason for new floaters to appear in the vision. While a retinal tear does not directly cause vision loss, it can serve as a pathway for fluid in the eye to travel through the tear and underneath the retina. Think of a retinal tear as a precursor to a retinal detachment.
If fluid from inside the eye does travel through the tear and underneath the retina, a retinal detachment occurs. When the retina becomes separated from it’s supporting layers in the back of the eye, it quickly degenerates and vision loss ensues.
I grew up in Miami where the name Baskin Palmer is golden. Finding Dr. Shane had studied at Baskin was a huge relief. My husband suffered a sudden detached retina so we had no time to waste. Dr Shane changed his schedule at the surgery center, having both the anesthesiologist and the staff stay to accommodate my husband.
The skill and dedication of this man is amazing! It’s been a year and a half since the surgery and we are so grateful Sam still has vision in that eye, yes it was that bad of a detachment. Dr. Shane has always been straight forward and explains choices in terms we can understand. We appreciate everything he has done for Sam!!!!!
The staff is also wonderful, so warm and welcoming, and willing to go the extra mile. I work in the healthcare field and know the good side and the bad. Dr. Shane and his staff remain good guys, skilled and knowledgeable, and above all caring and concerned. You are not just a number to them or a 15 minute visit. They care about you!
Did I Cause My Retinal Detachment?
 The separation of the vitreous jelly from the retina in mid-life is basically unavoidable. This spontaneous event will occur in most people regardless of trauma history, nutrition, or overall health. Similarly, whether the vitreous jelly separation causes a retinal tear or detachment is largely out of the control of most patients.
The separation of the vitreous jelly from the retina in mid-life is basically unavoidable. This spontaneous event will occur in most people regardless of trauma history, nutrition, or overall health. Similarly, whether the vitreous jelly separation causes a retinal tear or detachment is largely out of the control of most patients.
There are a few risk factors, however, that make a retinal detachment more likely. The first would be severe nearsightedness, also known as high myopia. In these patients, the eyeball is much larger than average, with corresponding thinning of the retina. Another risk factor is family history of an RD. Some inherited characteristics that make the jelly or the retina form detachments can be passed down through the generations.
Additional risk factors include previous eye surgery or severe ocular trauma. If you are found to have areas of thinning in your retina, called lattice degeneration or retinoschisis, you may be slightly more likely to develop a retinal detachment. Still, the vast majority of retinal detachments occur for no other reason than the structural limitations of the human eyeball.
The vast majority of retinal detachments occur for no other reason than the structural limitations of the human eyeball.
What Happens At My Eye Appointment for New Flashes and Floaters?
If you are experiencing new flashes, floaters, or grey curtain in your vision, you should schedule a dilated eye exam with an ophthalmologist within 24-48 hours. On the day of your appointment, you will have your vision, eye pressure, and peripheral vision checked by a technician. The pupils will be dilated to allow for a clear view of your entire retina. Retinal images will be taken using specialized cameras to detect the presence of a retinal detachment or other eye disease. Lastly, you will be examined by the ophthalmologist and the findings and treatment plan will be discussed.
I Have a Retinal Tear. How Do We Treat It?
If you are found to have a tear in the retina, but no detachment, you will likely undergo a retinal laser to seal the tear and prevent a retinal detachment. The laser works by creating a barrier of scar tissue around the tear, preventing fluid from inside the eye from traveling through the tear and underneath the retina. This procedure can be performed immediately in the office with mild discomfort and no permanent vision loss. Laser for retinal tear typically takes 5 minutes, with patients able to return to their normal activities later in the day.
Keep in mind that it takes at least 7 days for the laser to seal the tear, so you are still at risk for a retinal detachment over than time. In addition, a new tear may form elsewhere in the retina, which can progress to retinal detachment if left untreated. For that reason, it is important to report any onset of new floaters or loss of peripheral vision following your retinal laser.
Important disclaimer: the retinal tear laser is intended to prevent a retinal detachment. Laser for retinal tear does not specifically improve floaters that may be in your vision due to debris suspended in the vitreous jelly that fills the eye. Floater symptoms tend to improve on their own without treatment over the period of weeks and months.
I Have a Retinal Detachment. What Are the Options for Treating It?
Patients found to have retinal detachments should expect to undergo a surgical procedure to repair the problem. There are various options for treating a retinal detachment. The choice of which procedure to use depends on the characteristics of your RD and surgeon preference. Listed below are several options in rough order of least to most invasive.
Retinal Laser: In a minority of cases, a retinal detachment can be isolated with laser alone. The advantage of this treatment is that it can be applied immediately and non-invasively in the clinic. The disadvantage to retinal laser is that it doesn’t prevent progression of the retinal detachment until a week after treatment. For this reason, it is inappropriate for most new retinal detachments, but a reasonable option for those detachments that are chronic in nature.
Pneumatic Retinopexy: This procedure involves the injection of a gas bubble into the eye to flatten the retinal detachment along with laser or freezing treatment to seal the retinal tear. It works well with retinal detachments with single tears located near the top of the eyeball. The advantages to pneumatic retinopexy include that it can be performed same-day in the clinic and leads to slightly better visual outcomes than surgery. The disadvantages include a lower success rate (60-70%) and positioning requirements for ~7 days after the procedure.
Vitrectomy: This outpatient surgical procedure is the most common treatment for all types of retinal detachments. Performed at a hospital or surgery center, it can be accomplished in about 45 minutes using local anesthesia, with a success rate around 85-90%. During the procedure, the surgeon removes the vitreous jelly from the eye, replacing it with clear saline. The retinal is reattached and the tears are lasered from the inside of the eye. A gas or oil bubble is used to hold the retina in place until the laser seals the tears. Patients frequently have to take uncomfortable head positions for 7 days and avoid air travel for weeks following a vitrectomy for retinal detachment.
Scleral buckle: This outpatient surgical procedure was one of the first solutions to retinal detachments, dating back to the 1950’s. Success rates for scleral buckle are similar to vitrectomy, but require larger incisions and carry an increased risk for double vision and nearsightedness afterwards. On the other hand, the risk for cataract is much lower for scleral buckle than vitrectomy. For this reason, scleral buckle tends to be the procedure of choice for patients who develop retinal detachments before the age of 50.
How Soon Do We Treat a Retinal Detachment?
Most retinal detachments require some form of surgical repair within 1-2 weeks. The urgency of the repair depends on the extent of the detachment. If the separation of the retina has not yet progressed through the center of the vision (macula-on), the surgeon may schedule a procedure within 24-48 hours depending on surgery center availability. If the retinal detachment has already involved the central vision, then the timing of the procedure is usually 1-7 days after diagnosis with comparable visual outcomes.
Contact Us in Sarasota or Manatee County for Retinal Detachment Symptoms
Have you been experiencing new flashes of light, floaters, or sudden loss of vision? You may have a retinal detachment. We offer emergency retinal detachment surgery or laser treatments in Sarasota & Manatee County.
Our ophthalmologists located in Sarasota and Manatee County is specialized in managing retinal detachments. A retinal detachment is considered an eye emergency, and permanent vision loss is possible if treatment is delayed. If you are having the symptoms mentioned above, seek a prompt dilated eye examination with our practice immediately. There are effective surgical and clinical treatments for most retinal detachments, so don’t delay.
