Retinal Tear Treatment & Options
Your Local Ophthalmologist Specialized in Retina
Neighborhood Retina Care Doctors in Sarasota, FL
Retina Specialists Providing Treatment for:
Retinal Tear Treatment
The retina is the inner lining of the eyeball which senses light and sends these light signals to the brain to be interpreted as vision. Think of the retina like the wallpaper of your eyeball and the pupil as the window to let light into the room. For various reasons, people can develop retinal tears in this very thin tissue that could result in permanent loss of vision. The following information is designed to help guide you through the various causes and types of retinal tears and subsequent retinal tear treatment solution performed by retina specialists.
Causes Of A Retinal Tear
The traditional rhegmatogenous retinal tear is created when the vitreous humor (the “jelly” that fills the eye) separates from the retinal surface. This is known as a Posterior Vitreous Detachment (PVD). The vitreous will often start its separation in the center of the eye (at the optic nerve and macula) and progress out to the peripheral retinal where the vitreous originates. When the vitreous pulls on the peripheral retinal (which is significantly thinner than the central retina)–a retinal tear can occur. Some individuals who have lattice (thin spots in the peripheral retina) have an increased risk of a retinal tear and detachment when the vitreous humor separates.
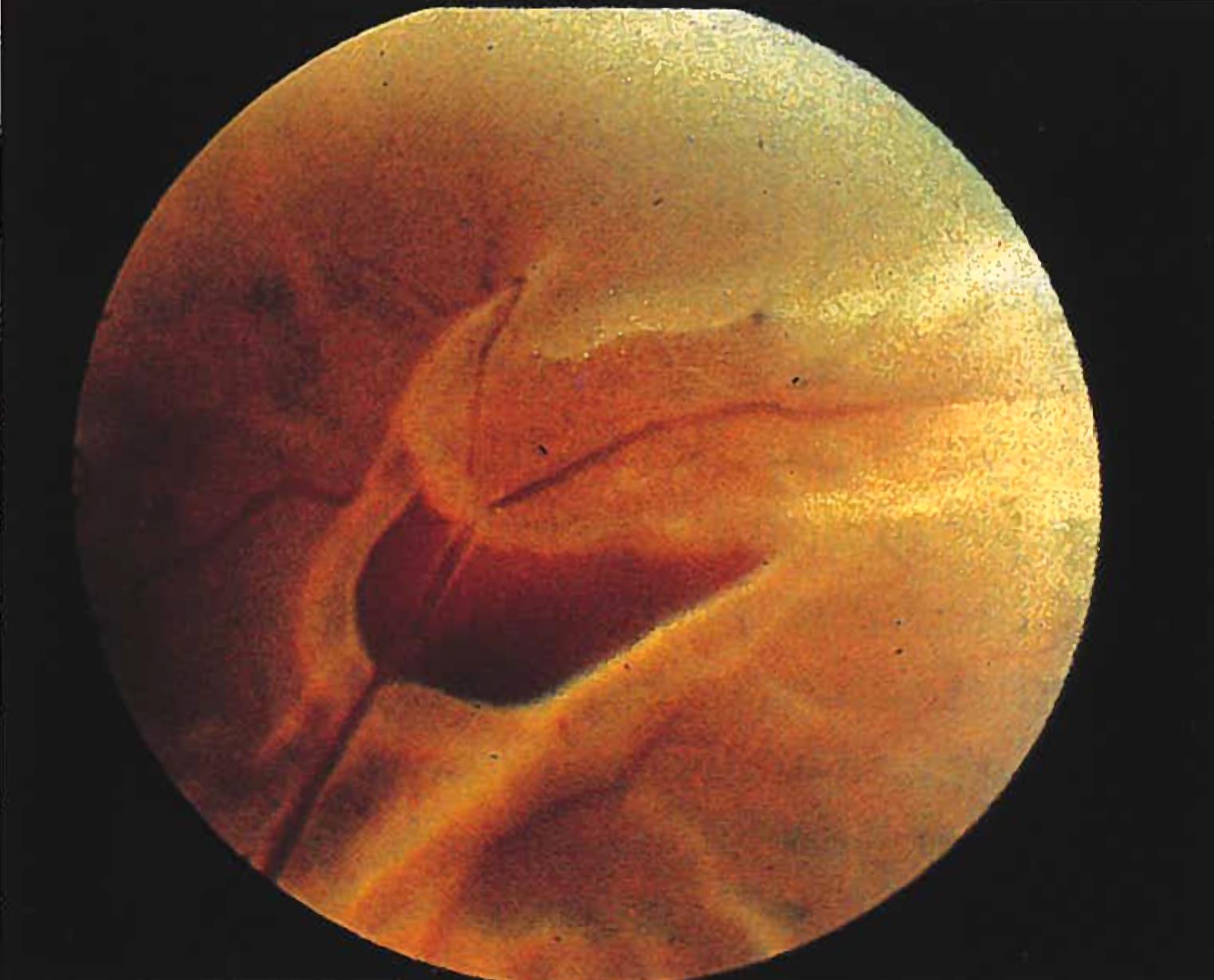
A tear in the retina can be categorized based on its appearance during a clinical exam by an ophthalmologist. There are three main types of retinal tears: an operculated tear (small circle of tissue torn out of the retina), a horseshoe tear (a ‘U’-shaped flap is lifted up), or a Giant Retinal Tear (a tear involving greater than 25% of the retina).
Risk Factors for Retinal Tear
- Severe nearsightedness
- Pre-existing thinning of the retina called lattice degeneration
- Prior eye surgery
- Advanced Age
- Trauma to the eyeball
- Previous Retinal Tear in the Other Eye
Symptoms Of A Retinal Tear
A retinal tear has similar symptoms of those with a posterior vitreous detachment. As the vitreous separates from the retina, it can cause a variety of symptoms, including new flashes or floaters. A retinal tear also causes flashes and floaters, and is indistinguishable from a vitreous detachment without a dilated examination. In a percentage of patients, there will be no symptoms and retinal tears may be discovered during routine examination by ophthalmologists. The following are a more detailed description of the common symptoms of PVDs/retinal tears:
Floaters – Patients may experience an increase in floaters–both large and small. The large floater is sometimes referred to as a Weiss Ring which is a piece of collagen that has pulled off from around the optic nerve giving it a ring appearance. Also, patients may perceive many small black dots sometimes described as black pepper flakes in the eye. These tiny floaters can be blood or pigment cells that have been released from the retina when a tear is present. Only a careful dilated eye examination can determine the origin and cause of the floaters.
 Flashes of Light – The retina is a neurosensory tissue designated to sense light and send those signals to the brain. When physically irritated by traction from the jelly in the eye, the retina will send false signals of light to the brain. The patient will perceive flashing light or “lightning bolts” in their vision. These flashes can be blamed on the normal, spontaneous separation of the vitreous jelly as it peels off of the retina or possibly a retinal tear. Either way, when a patient is experiencing new flashes of light, the best way to determine if there is a retinal tear or detachment is to have an ophthalmologist perform a dilated exam of the peripheral retina.
Flashes of Light – The retina is a neurosensory tissue designated to sense light and send those signals to the brain. When physically irritated by traction from the jelly in the eye, the retina will send false signals of light to the brain. The patient will perceive flashing light or “lightning bolts” in their vision. These flashes can be blamed on the normal, spontaneous separation of the vitreous jelly as it peels off of the retina or possibly a retinal tear. Either way, when a patient is experiencing new flashes of light, the best way to determine if there is a retinal tear or detachment is to have an ophthalmologist perform a dilated exam of the peripheral retina.
Curtain of Blurred Vision – If a retinal tear has formed, ocular fluid can begin to migrate through the retinal tear and under the retina causing a retinal detachment. These detachments will originate in the peripheral retina and are often not visually significant. However, as more fluid accumulates under the retina propagating the detachment, patients will notice a dark curtain of blurred vision opposite of where the retina is detaching. These symptoms require urgent examination to determine the cause of the loss of vision before retinal tear treatment.
Complications Of A Retinal Tear
Over time, the vitreous jelly that fills the eye becomes less like jelly and more like water. During this degradation, the vitreous can peel off of the retina and cause tears. Subsequently, the water that fills the eye can go through the tear and under the retina causing a retinal detachment. Referring back to the previous analogy, the eye is like a fluid-filled room with the retina being like the wallpaper in the room. If a tear existed in the wallpaper, fluid could seep underneath it. If enough water got underneath the wallpaper, it would start to peel off and detach. The same is true for the retina. Early recognition of a tear and prompt retinal tear treatment can prevent a large retinal detachment requiring invasive surgical repair.
Treatment Of A Retinal Tear

If identified early, a retinal tear can be treated with an in-office procedure. The two mainstay treatments for retinal tear are laser and freezing (cryopexy).
Laser: The retina can be treated to seal the borders around a retinal tear using a laser. The laser energy is absorbed by the retina, creating a tiny burn that scars the retinal layers together. This “weld” prevents any fluid from passing through the retinal tear and under the retina. The laser creates an adherence of the retinal layers that will be ultimately healed in 1-2 weeks. Laser cannot be successfully used if the retina is already detached, which is why surgery is usually the preferred treatment for retinal detachment.
Freezing (Cryopexy): Using a specialized probe, the retina specialist will freeze the tissue through the eye wall, creating inflammation and eventually scarring of the tissue to close the retinal tear. Similar to laser, freezing treatment results in no immediate adherence of the retina and will take time for the healing process to finalize. This can be an uncomfortable process, and some clinicians will elect to perform a numbing injection prior to treatment.
Note that both of these techniques can be used with attached retina. If there is fluid under the retina (a retinal detachment), the laser or freezing can be applied in combination with other procedures to attach the retina simultaneously. To reattach the retina in the office, a gas bubble is injected into the eye and placed over the retinal tear by having the patient position their head for 1-3 days. The fluid under the retina will be absorbed through natural retinal fluid pumps. Thereafter, the retina can be treated with laser or freezing. If there is a very large or complex retinal detachment, surgery is then recommended to reattach the retina and then apply laser at the same time.
Conclusion
Retinal tears may not be common in the general public, however, they are common enough to keep retina specialists busy. Holes in the retina need to be appropriately identified and treated in a timely manner. The retina specialists at Shane Retina are trained to identify retinal tears and detachments and administer office lasers, gas bubbles, and sometimes surgery the same day. If you are experiencing new floaters, flashing lights, or blurred vision, please make an appointment with your retinal specialist.
