Diabetic retinopathy is a complication of diabetes that affects the eyes. This condition can develop in anyone who has type 1 or type 2 diabetes. Diabetic retinopathy is defined as damage to the blood vessels located within the retina – the light-sensitive tissue of the back of the eye. Diabetic retinopathy has two main stages, nonproliferative and proliferative. However, these two stages can be further broken down into four distinct stages. Mild Nonproliferative, Moderate Nonproliferative, Severe Nonproliferative, and, Proliferative retinopathy. The longer you have diabetes and the less control you have on your blood sugar puts you at a higher risk of developing diabetic retinopathy.
The Four Stages of Diabetic Retinopathy:
Too much sugar in the blood can lead to blockage of the blood vessels that supply the retina, ultimately cutting off its blood supply. The eye in response will attempt to grow new blood vessels. These rogue blood vessels do not develop properly and can begin to leak over time. Each stage of diabetic retinopathy elicits different warning signs but builds on one another.
- Mild Non-proliferative Retinopathy – the first stage of diabetic retinopathy that is the hardest to recognize. Symptoms within this stage are mild but may include an increase in blurred vision. Blurred vision in this stage is caused by small bulges in the blood vessels of the retina. The bulges are known as microaneurysms that may result in leakage of the blood vessels. It is important if you are in this stage of diabetic retinopathy to control your blood sugar and have your eyes checked every 12 months. Proper management of blood sugar can delay the development of complications.
- Moderate Non-proliferative Retinopathy – In this stage, blurriness becomes more apparent, and your visual acuity may begin to decline. The blood vessels within the retina begin to swell causing changes to the retina. These physical changes to the retina may lead to diabetic macular edema (DME). Diabetic macular edema is when fluid begins to build up in the central-most region of the retina – the macula. The macula is responsible for your central pinpoint vision. Swelling in this portion of the retina will affect your vision. Patients who have reached this stage will need to be monitored more frequently to preserve their vision. Your ophthalmologist may recommend eye exams every three to six months.
 Severe Non-proliferative Retinopathy – The third stage of diabetic retinopathy is also known as pre-proliferative retinopathy. In this stage, the blood vessels in the retina are blocked, significantly reducing the amount of blood going to the retina. This prevents the retina from functioning properly and triggers a protein called VEGF to create new blood vessels. In this stage, vision may decline, and you may lose the ability to properly see at night. Additionally, you may see an increase in floaters or dark spots in your field of vision. Reaching this stage puts you at high risk of permanent vision loss. Treatment will be necessary to slow the progression of further vision loss.
Severe Non-proliferative Retinopathy – The third stage of diabetic retinopathy is also known as pre-proliferative retinopathy. In this stage, the blood vessels in the retina are blocked, significantly reducing the amount of blood going to the retina. This prevents the retina from functioning properly and triggers a protein called VEGF to create new blood vessels. In this stage, vision may decline, and you may lose the ability to properly see at night. Additionally, you may see an increase in floaters or dark spots in your field of vision. Reaching this stage puts you at high risk of permanent vision loss. Treatment will be necessary to slow the progression of further vision loss.
- Proliferative Diabetic Retinopathy (PDR) – The final and most advanced stage of diabetic retinopathy is very serious. Large areas of the blood vessels in the retina are obstructed preventing the retina from receiving proper nutrients to function. Patients may notice a reduction in their peripheral vision at this stage. In this stage, the retina grows new blood vessels to compensate for the lack of blood flow. This is known as neovascularization. These weak vessels may bleed into the gel-like fluid that fills the eye (the vitreous). Bleeding into the vitreous is known as a vitreous hemorrhage. Vitreous hemorrhage can cause an increase in dark floaters or complete blockage of vision. Additionally, these blood vessels may form scar tissue on the retina leading to a retinal detachment. Vitreous hemorrhage and retinal detachments cause significant loss of vision.
Risk Factors of Diabetic Retinopathy:
Anyone with type I or type II diabetes is at risk for developing diabetic retinopathy. This includes those who develop diabetes during pregnancy (gestational diabetes). The risk for developing diabetic retinopathy increases for those who have:
- Poor control of blood sugar levels
- Prolonged diabetes
- High blood pressure
- High cholesterol
- Prolonged use of tobacco
What Complications are Associated with Diabetic Retinopathy?
Due to the growth of abnormal blood vessels in the retina, complications of diabetic retinopathy can have serious effects on your vision. This includes:
- Vitreous hemorrhage: The vitreous is the clear gel-like fluid that fills the center of the eye. As new blood vessels grow in the retina, they may begin to bleed into the vitreous. This bleeding may cause you to see new dark floaters, or in more severe cases, a complete blockage of vision. Unless the retina is damaged, the blood usually clears on its own in a few weeks or months. In some cases, surgical intervention to clear the blood may be necessary.
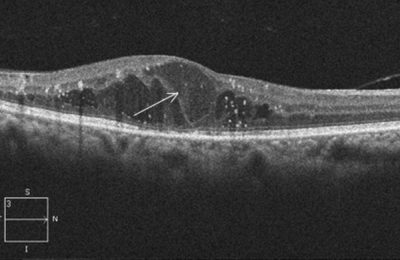
- Diabetic Macular Edema (DME): A condition in which fluid accumulates causing swelling in the macula. This is caused by leakage of abnormal blood vessels in the retina. This condition causes distortion of vision and if left untreated may lead to permanent vision loss. Treatment may include intravitreal eye injections or laser treatment to prevent the blood vessels from continuing to leak.
- Retinal Detachment: Proliferative diabetic retinopathy (PDR) may cause scars to form on the retina. If this occurs, the scars may pull your retina away from the back of the eye causing a tractional retinal detachment. Surgical intervention may be necessary to reattach the retina and prevent permanent vision loss.
How To Prevent Vision Loss from Diabetic Retinopathy?
Properly managing your diabetes is key in preserving your vision. If you are a diabetic, it is important to:
- See your ophthalmologist for regular dilated eye exams. If diabetic retinopathy is found in its early stage, your ophthalmologist will be able to properly monitor your condition before further vision loss occurs.
- Talk to your primary care doctor about appropriately controlling your blood sugar. Increased blood sugar causes damage to the blood vessels in your eye and can lead to vision loss.
- Consult your ophthalmologist immediately if you notice any changes to your vision.
- Controlling your blood pressure and cholesterol levels.
- Discontinue any tobacco use.
Taking an active role in managing your diabetes is important. Having diabetes does not necessarily lead to loss of vision. Consulting your ophthalmologist and primary care physician in managing your diabetes can aid in the prevention of diabetic complications.

 Are you experiencing vision issues and not sure what is happening? At Shane Retina, we are retina specialists equipped to deal with the full range or retina issues. Contact us today to get help now!
Are you experiencing vision issues and not sure what is happening? At Shane Retina, we are retina specialists equipped to deal with the full range or retina issues. Contact us today to get help now!